Purpose of Curriculum
1. Draws from the strengths and professional expertise of both disciplines,
2. Bridges the gaps between the systems by creating a unified and comprehensive treatment approach, and
3. Provides substantially improved outcomes for those presenting at mental health or addiction treatment facilities.
The terms “best practice standards” and more recently “evidence based practices” have become a part of our daily vocabulary. Fully integrated services have been identified as both evidenced based practices (EBP) and best practice standards by distinguished organizations, as well as individual experts and groups of experts throughout the United States and internationally. To name just two of the groups identifying integrated treatment as (EBP) included:
- SAMHSA (Substance Abuse and Mental Health Services Administration) has recognized the CCISC Model (Comprehensive Continuous Integrated System of Care), designed by Kenneth Minkoff, M.D. and Chris Cline, M.D., as EBP for systems implementation for the treatment of ICOPSD (integrated treatment of individuals with co-occurring psychiatric and substance disorders).
- The Report of The Center for Mental Health Services Managed Care Initiative: Clinical Standards and Workforce Competencies Project Co-Occurring Mental and Substance Disorders Panel (a panel of nation-wide experts) called for the integration of services in their final report “Co-Occurring Psychiatric and Substance Disorders in Managed Care Systems: Standards of Care, Practice Guidelines, Workforce Competencies, and Training Curricula” (1998), Panel Chair Kenneth Minkoff, M.D.Drawing from each of these bodies of expertise, clinicians are urged to develop basic knowledge of psychiatric and substance disorders and their interactions, and the skills to be able to consistently demonstrate familiarity with an integrated disease and recovery model. The goal of providing quality psychoeducational material is addressed within these reports, as well as from many other sources, not to mention our own ethical standards of service delivery.
Challenges
Most therapists have been primarily trained along one track, either in mental health disorders or substance use disorders. The integrated system approach recommended that each field to provide simultaneous psychiatric and addiction treatment. Service providers and program curriculum designers often find this a daunting task. Even though availability of cross-training is expanded, the ability of most providers to revamp their current curriculum continues to be limited due to their current caseloads, cost or budgeting restrictions, or constraints on staff and other resources.
The importance of a consistent agency-wide curriculum or body of psychoeducational material can’t be overstated. All sources of EBP speak to the importance of consistency. This is especially true when working with people whose very symptoms rob them of consistency either in their moods, thoughts, or behaviors. Whether psychoeducational material is presented primarily in group, is used mostly to guide treatment planning, is discussed predominantly in 1:1 sessions, or is beneficial for cross-training mental health and addiction professionals – it must be consistent among service providers – especially within the same treatment setting.
When treatment and education are consistent, treatment participants benefit from interacting with a treatment team that is cohesive. The material covered in group then filters into questions and areas of exploration in 1:1 sessions and subsequently guides treatment planning as well as case management.
My personal experience in treatment facilities ranges from agencies where no curriculum was available because senior staff had developed a sort of rolodex of vast knowledge “in their head” that resulted in me spending endless hours trying to glean their knowledge in a way that was usable to me personally; to agencies where sparse outlines were available with stated objectives like “teach biochemistry of addiction” that also resulted in spending hours sitting in on other groups to “catch on” to the full intent and meaning of the outline; to agencies where skilled clinicians had psychoeducational material in their desk drawers that was not available to the rest of the staff or the entire treatment population for that matter.
When it came to a curriculum being available in any form to provide consistent psychoeducational material in the area of dual diagnosis; well, that was another story altogether. Agencies were working back and forth literally between pieces of material gathered from books, literature, and the internet. When I began to facilitate groups for the dually diagnosed using a consistent curriculum I had developed for my own use, I gradually ended up with more therapists in my groups than group members!
The therapists told me they wanted to sit in on the groups because the individuals in treatment kept drawing the same pattern on a piece of paper. The therapists said, “When they come in for their 1:1 sessions they want me to see something that is really helping them.” The therapist would then show me the drawing and ask, “What is this? People in treatment say it helps them to really understand that their illness is truly not their fault. They now fully know they are not ‘bad’ or ‘weak.’ They feel hopeful that treatment will give them the information to help themselves!” I got so many requests that I could answer the question without looking at the drawing. “Well, that is neurotransmission and we talk about biochemistry of dual disorders in one of the psychoeducational groups.”
As I watched therapists and group facilitators furiously taking notes, I realized the consistency between groups would probably depend on how well each therapist took notes or how well key points were remembered later. The idea of writing out the material in a very detailed, comprehensive form was born.
A Solution
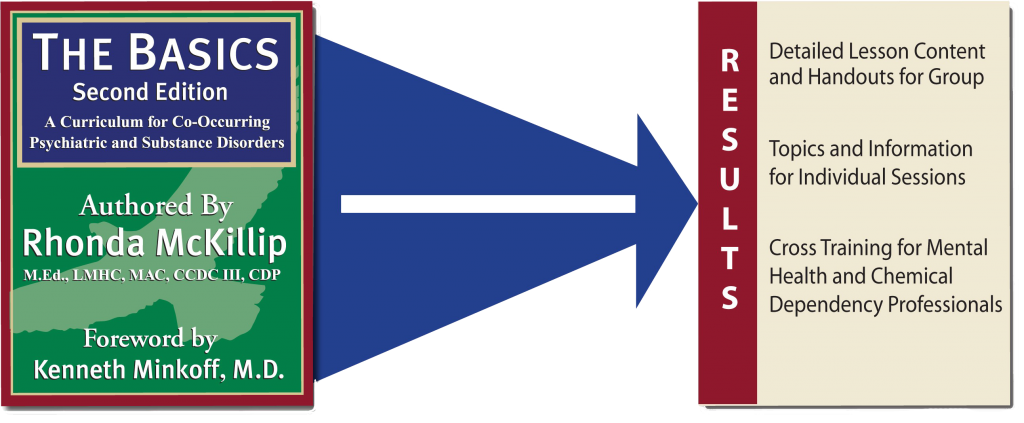
Develop a comprehensive, integrated curriculum that meets the needs of the dually diagnosed population and provides consistent psychoeducation throughout the treatment setting in a format that simultaneously includes:
- Detailed Lesson Content and Handouts for Group
- Topics and Information for Individual Sessions
- Cross-Training Guide for Mental Health and Chemical Dependency Professionals
Additionally, the goals of the curriculum are to:
- Meet the needs of people with psychiatric and substance disorders at various levels of severity, chronicity, and acuity.
- Reduce or eliminate the endless hours professionals spend on creating their own group or 1:1 psychoeducational material.
- Create a concrete avenue to cross-train therapists in integrating psychiatric and substance disorders treatment.
- Provide substantial bibliographies on each subject to create a substantial reference guide, as well as to enhance the confidence of the individuals in treatment and the professionals.
- Make available a substantial amount of curriculum material to allow flexibility for any number of treatment groups offered in various treatment settings.
- Promote self-efficacy as treatment participants are encouraged to gauge their own readiness for change, along with specific tools to work through ambivalence.
- Provide interactive handouts for each subject designed to engage the group members in discussions.
- Eliminate the need to use hard-to-read, uninteresting, multi-generational handouts by providing handouts with graphics, information, and subjects to promote group interaction.
- Allow group members to personalize the material, internalize the subject matter, and interact with other group members – all essential ingredients in the process of change.
- Reduce the need for group facilitators to take notes or research key points in material presentation by incorporating “Tips to Professionals” into the program curriculum.
- Incorporate in the curriculum language – from beginning to end – the principles of hope and empathy, as well as consistency of information presented in an interactive format into the treatment program itself.
Welcome to THE BASICS, Second Edition!